Dental billing can be an overwhelming task thanks to continually updated CDT codes, ever-changing insurance regulations, and rapid advancements in dental technology. When you add in specialty treatments like endodontics, orthodontics, and periodontics, it can be even more overwhelming and you may not even know where to begin. But, with a little guidance, specialty dental billing can become much less intimidating and much more manageable. In this ongoing series, we will offer insight into the various nuances of specialty billing practices beginning with periodontal billing.
What is Periodontics?
Periodontics is the treatment of the tissues supporting the tooth, such as the gums and jawbone. Depending on the circumstances, this treatment can be completed by a dental hygienist or a periodontist. According to the American Academy of Periodontology, a periodontist “specializes in the prevention, diagnosis, and treatment of periodontal disease…and in the placement of dental implants.”
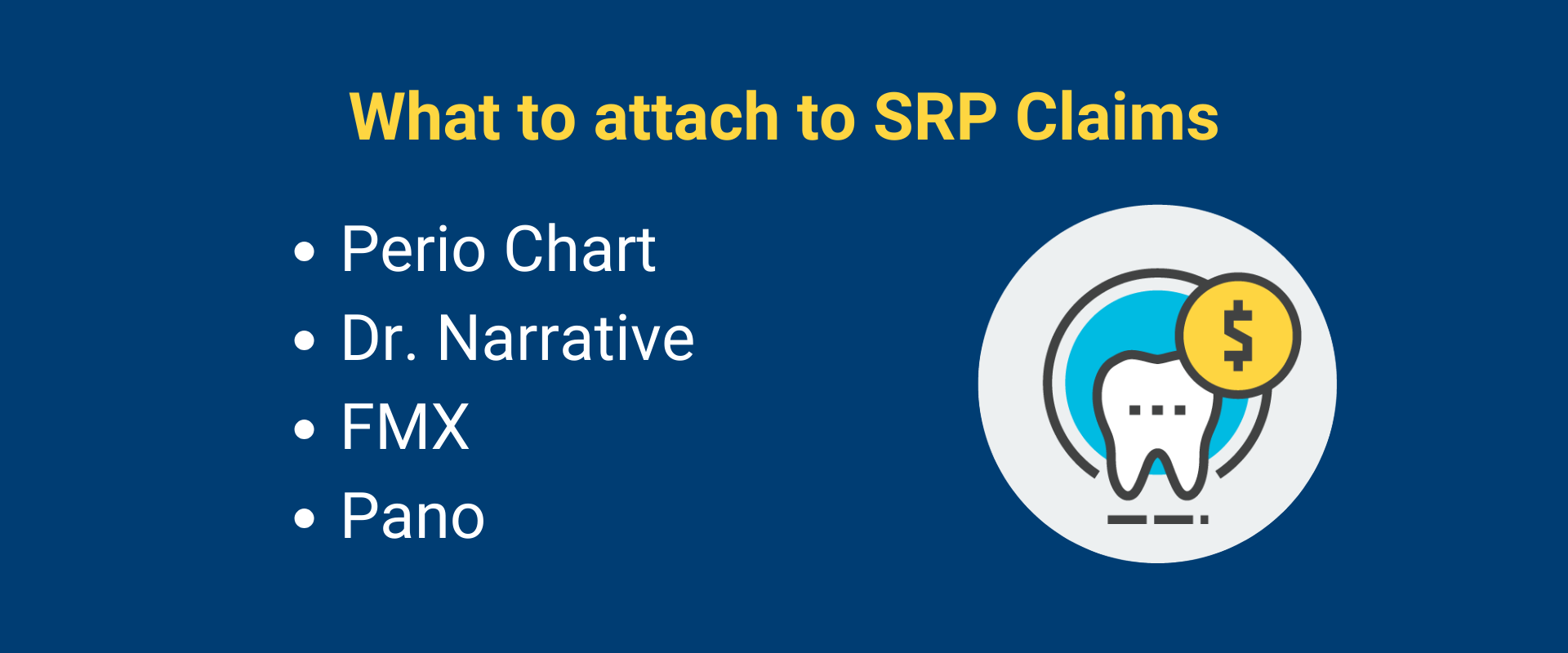
What attachments do I need to include in a periodontal claim?
When billing periodontal treatment, the attachments vary from procedure to procedure but at the very least include x-rays, a clinical narrative, and a periodontal chart. The x-rays should show the affected area and, when possible, include both full mouth (FMX) and panoramic, especially when billing scaling and root planing (SRP). Also, when billing SRP, it helps to include the length of treatment time as some insurances are starting to require this. If billing perio maintenance, be sure to include the date of the previous SRP and/or maintenance. For implants, include the date the tooth was extracted, and for bone grafts, include the implant treatment plan, if it applies.

Do I need a referral?
When billing a PPO insurance, you don’t need a referral but it may be required for an HMO plan. If the treatment was completed by a hygienist, a referral isn’t necessary but if it was completed by a periodontist, the HMO plan won’t consider the claim without it. Some carriers do require treatment to be pre-authorized, especially when implants are completed. Always check when verifying insurance coverage if it is required.
How do I bill scaling and root planing?
When billing SRP, it’s essential to provide as many details as possible in the claim. If billing D4341 (4 or more teeth per quadrant) be sure to include the quadrant treated, and, if billing D4342 (1-3 teeth per quadrant) be sure to include the specific tooth numbers treated. Attachments must include a recent perio chart, x-rays (ideally FMX and pano), and a clinical narrative that addresses the pocket depth and any bone loss. It also is best to include the length of treatment time.
Why was my scaling and root planing claim denied?
Currently, insurance carriers are growing suspicious of upcoding when it comes to SRPs and they are frequently denying them. Most carriers have strictly regulated the circumstances in which they allow coverage and no two carriers are alike. For instance, each insurance carrier has a specific pocket depth requirement for scaling and root planing and none allow less than 4mm. In fact, several carriers are now requiring 5mm or more. In addition, most require evidence of bone loss and without it, they won’t consider payment. Also, some carriers only allow 2 quadrants per visit and if 4 are completed, the additional 2 won’t be covered, except in rare circumstances. Confirming insurance requirements when verifying coverage is essential if you want to get your claim paid. Consider outsourcing insurance verification, if you’re struggling to find the time to do this.
What is the difference between prophy and perio maintenance?
Prophylaxis is the removal of plaque, calculus, and stains from teeth whereas perio maintenance is a slightly more extensive cleaning that is exclusively used on patients who have had previous periodontal treatment. According to the ADA, perio maintenance can continue through the life of the teeth but most insurances cover a much shorter period. Generally, they will only cover it within 24 months of SRP treatment, and, in addition, most limit coverage to once every 6 months. Sometimes, they will consider an alternative benefit downgrade of prophy but, often, they will simply deny the treatment if the frequency limits are met.
Are implants covered by insurance?
It all depends on the insurance plan. At one point, they were rarely covered, as they were considered a cosmetic treatment, but now there’s a better chance of some payment. Some carriers will cover adjunctive treatment, like bone grafts, but not the actual implant. Others may cover it at an alternative benefit downgrade of a denture. If the plan does cover it, verify if a missing tooth clause applies. If it does, and the tooth was extracted before the plan was effective, the implant will be denied.
As you can see, many different circumstances arise when billing periodontal treatment, and, though manageable, it can take up a large portion of the dental billing process. If you’re struggling to find the time to allow for this, consider outsourcing your dental billing. At eAssist, the Success Consultants who use our platform are knowledgeable about the various nuances of periodontal treatment and will ensure your claim is billed correctly. To learn more, complete the form below.








0 Comments