Dealing with dental insurance requires knowledge, patience, and the ability to see past the bizarre. The constant insurance changes are a lot to keep up with, sometimes even for insurance carrier representatives. We have compiled some of the worst, wildest, and wackiest dental billing claim stories from 2021 from our eAssist Success Consultants. Enjoy!
Missing tooth clause
There was a patient that came in for an extraction in December 2019 and was scheduled for an implant in April 2020. Obviously, the appointment to place the implant was canceled due to COVID-19. In December 2020, her employer switched insurance companies. She was finally able to come in to place her implant in May 2021 and have the implant crown placed in September 2021. The new insurance denied both claims due to a missing tooth clause. The office manager told me not to worry about appealing, but I sent an appeal explaining the situation anyway. It wasn’t the patient’s fault and the insurance should pay! I’m still waiting for a response.
I had a claim for a patient that had been in dentures since he was a teenager, due to an accident involving a tractor that caused severe blunt trauma to his face. He is now in his 50s and was needing to replace his dentures of 20 years. Well, his insurance ended up denying the claim stating they had a missing tooth clause. While this is pretty common for insurances, this patient was not aware that he was paying for dental insurance that wouldn’t cover him. They allowed him to pay for insurance but refused to cover any treatment because he didn’t have any teeth when he enrolled. The worst part? The patient said he told the representative that signed him up for coverage that he didn’t have any teeth! I gave the insurance company two options: 1) refund the patient for 10 years of dental coverage or 2) pay for new dentures. After 13 months of back and forth, they paid the claim. The patient canceled coverage shortly after.
Simple misunderstandings
I called regarding a request from an insurance payor for information that we had included on the NEA. The representative informed me that the data I had submitted was unclear. I went back and forth until she says, “The whole submission is fuzzy.” Now I’m getting frustrated because I thought it was very obvious. Finally, she says, “Well, everything is blurry.” I said, “Quit with the metaphors!” Nope, she literally meant that everything was blurry and she couldn’t read it. The whole conversation finally made a lot more sense!
Recently an insurance payor interpreted the $150.00 amount on the claim as $1.50. They did this for each of the procedures, so I received a payment of $6.00.
I had an office manager call me and tell me that a patient wanted his deductible billed to his insurance because refused to pay it. He felt his insurance should pay the deductible. I spent 10 minutes explaining how the deductible is the patient’s responsibility. The worst part? The patient was a doctor!
Wild and wacky
I had a call yesterday that a single crown was denied because the patient “has too many teeth.” The representative told me if there are more than 8 points of contact, then they won’t pay for a crown. Was she serious? I had her clarify that 3 times. Strangest denial I’ve ever heard.
With most of the insurance representatives working from home in 2021, I’ve heard the strangest things in the background when calling about claims. Roosters, elephants, you name it! Most recently, a rep was taking a long time to answer my questions. She finally got up to speed after I heard the toilet flush! She was a very kind representative and ended up helping me with ALL of my claims for that payor. I would have remembered her for her kindness and friendly conversation, but now I couldn’t flush the memory if I wanted to!
I called an insurance company to get a breakdown of benefits for a patient. I asked if composites were covered on posterior teeth or were they downgraded? The representative gets very serious and says, “Posterior? Do you mean the butt? How do I check that?” I couldn’t stop laughing. I finally stopped long enough to say, “Not that posterior, the BACK teeth!”
Had a patient that was 107 years old that came in for new dentures. The insurance denied her panoramic x-ray because she “was over the age limit of 99.” That was a fun one to appeal.
Dental billing claims experts
The insurance carrier landscape is constantly evolving, and it can be hard to keep up. Just take a look at what dental administrators have to stay up-to-date on every year:
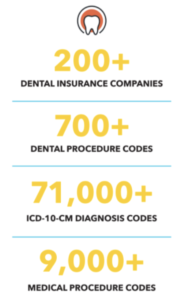
Just in 2022, there are 16 new codes, 6 deleted codes, 14 revised codes, 10 editorial revisions, and 8 updated codes. Feeling overwhelmed? We understand and are here to help. At eAssist, our Success Consultants have over 10,000 YEARS of combined dental billing and insurance experience. We can help you navigate the worst dental billing claims in your office! Click here to set up a complimentary consultation.







0 Comments